Treating IBD
with Immunotherapy:
The MITI2 Promise
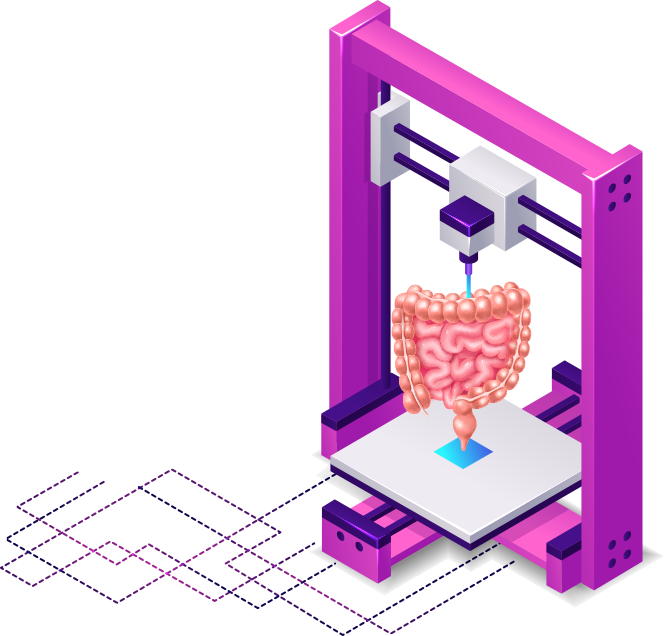
MITI2 program works on a novel cell-based immunotherapy approach for patients with Inflammatory Bowel Disease, thanks to an original ex vivo human preclinical model and an innovative bioprinting method.
There is a need for additional safe and effective therapeutic options to address unmet treatment needs for patients with Inflammatory Bowel Disease (IBD). Emerging therapeutic options like immunotherapy and cell-based therapy are particularly promising strategies in IBD.
P1a-INSERM has recently identified a novel microbiota-induced Treg subset, associated with unprecedented clinical outcome of IBD patients.
Immunotherapy is a type of medical treatment that harnesses the power of the body’s immune system to combat diseases, particularly those related to the immune system itself, such as autoimmune disorders, infectious diseases or cancer. The immune system is a complex network of cells and proteins that work together to defend the body against harmful invaders, such as bacteria, viruses, and abnormal cells. There are several different approaches to immunotherapy, including Immune checkpoint inhibitors, Monoclonal antibodies, Cancer vaccines, Adoptive cell transfer and indeed CART-T Cell therapy.
MITI2’s main objective is to deliver an innovative immunotherapy approach using the regulatory properties of this gut microbiota-specific regulatory T (Treg) cell subset.
About IBD
A disabling chronic inflammatory process
Affects young
individuals
Causes many life-altering symptoms as well as life threatening complications
Severe abdominal pain, diarrhea, nutritional deficiencies, weight loss
Fistula/perforation, obstruction, colorectal cancer
IBD includes Crohn’s disease (CD) and ulcerative colitis (UC)
A total cost of €990 million per year for the French Health Care Insurance*
IBD cannot be cured at the moment, life-long treatments are the unique medical solution to date for a stable control of the disease, for non-evolutive forms.
*A total cost calculated in 2017 including more than €480 million for city care and more than €430 million for hospital care
Challenges
A high rate of anti-TNFs treatment failures
The last 2 decades have seen many advances in the therapeutic landscape, with mainstream use of antitumor necrosis factor (anti-TNF) agents. However, treatment failure occurs in a significant proportion of patients treated with anti-TNFs. Approximately 50% of patients will not respond to initial treatment (primary nonresponders), and 40% of responders will fail to respond at some point during the disease course (secondary nonresponders). Additionally, the benefit of anti-TNFs is tempered by serious adverse effects.
A benefit-risk unknown with new treatments
Multiple new drugs targeting various aspects of the pathophysiology of IBD have therefore been developed. Although the availability of these therapies has greatly improved the outlook for IBD management, it is important to remember that many of the agents are new or still in the development pipeline, and the benefit-risk balance should be actively considered when making treatment decisions.
A human physiological complexity to reconstitute for research validation
Based on the limitations to develop immunotherapy approaches for human diseases using animal models, MITI2 program opted for the development of an ex vivo human preclinical model that will reconstitute the physiological complexity of the human gut including dynamic interactions between the gut epithelial cells, the immune cells/lymphoid structures and the enteric neuronal/glial ganglia.
A dynamic interactions tissue model setup only at its beginning
Based on the limitations to develop immunotherapy approaches for human diseases using animal models, MITI2 program opted for the development of an ex vivo human preclinical model that will reconstitute the physiological complexity of the human gut including dynamic interactions between the gut epithelial cells, the immune cells/lymphoid structures and the enteric neuronal/glial ganglia.
A world-renowned expertise needed
So far, only attempts to associate epithelial gut organoids with immune cells or enteric ganglia have been done and are still to be improved. They have also been identified as a high priority to investigate the impact of drugs on the gut. There is no evidence in the literature that multi-tissues gut ex vivo models that associate the epithelial layer with immune cells, neuronal/glial enteric structures and vascularization have been yet developed. MITI2 with partners expertise in the epithelial gut organoid’s, the world-renowned expertise in ex vivo models of neuronal/glial enteric structures, and in the ex vivo models of immune structures, tackle this challenge.
Ambitions
1
An immunotherapy product
Ready to be used
in a phase 1
of clinical trials
2
A preclinical package
A. The proof of concept of a cellular immunotherapy clinically suitable for IBD patients treatment.
B. An original gut-explant-based organoid preclinical model.
An organoid is a three-dimensional, miniature organ-like structure that is grown in a laboratory from cells, typically stem cells or tissue-specific cells. Organoids are designed to mimic the structure and function of real organs in a more simplified and controlled environment. These structures can be used for various purposes, including studying organ development, disease modeling, drug testing, and personalized medicine.
While organoids have great potential, there are still challenges in replicating the full complexity of real organs, and improvements are continually being made in terms of their maturity and functionality. Overall, organoids have become a critical tool in biomedical research, offering a bridge between traditional cell culture and in vivo animal models. They provide a more accurate and ethical way to study organ function and disease processes, and their applications are continually expanding.
Innovation in MITI2
A bio manufacturing method, as a premiere in producing complex 3D structures such as the gut and its environment.